On 20 August, 2020, the world-famous journal Nature formally published the latest study result Reconstruction of the full transmission dynamics of COVID-19 in Wuhan by School of Public Health of HUST. This study further evaluated the effect of control strategies through a mathematical modelling and showed the transmission features of COVID-19 based on the JAMA paper published in April summarizing the correlation between public health interventions in Wuhan and the epidemic trend. It will contribute to the more effective formulation of prevention policies and programs of all countries around the world and guide China to achieve the ultimate victory in the fight against the epidemic and fight against potential new infectious diseases in the future. It has attracted widespread attention since its online publication on 16 July, 2020.
The study extended the classic SEIR model to a SAPHIRE model for fitting and parameter estimation of the epidemic curve of Wuhan as of 8 March by combining the known features of novel coronavirus pneumonia (COVID-19), including infectiousness before the onset of symptoms, the undetectable of a large number of infected people due to mild symptoms, and the relatively weak infectiousness of mildly symptomatic patients, and considering the varying population movement and intervention strength in different stages. By model comparison, the study observed that multipronged interventions taken after Wuhan lockdown since 23 January, 2020 reduced the total infections in Wuhan by 96.0% as of 8 March, 2020; centralized isolation of “four types of people” since 2 February cut the number by 69.6% (Fig.1). These results reflected the remarkable effect of joint prevention and control, which greatly protected the life and health of the people.
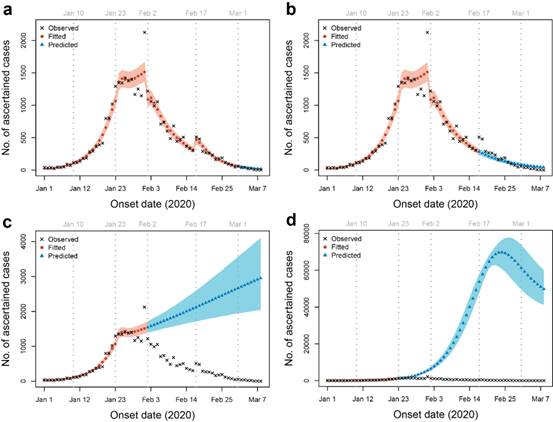
Fig.1. Trend fitting and prediction of daily onset patients under different conditions: (a) Fitting of the actual situation; (b) Trend prediction if without universal screening after 17 February; (c) Trend prediction if without measures such as centralized isolation after 2 February; (d) Trend prediction in the case of no intervention at all.
The modelling identified two key features of the outbreak: high covertness and high transmissibility. There was a basic reproduction number (R) of 3.54 in the early outbreak, much higher than that of severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). R decreased significantly to 1.18 since the intervention measure from 23 January, with daily onset number slowing down; R further decreased to 0.51 since centralized isolation after 2 February, with daily onset number decreasing day by day; R decreased to 0.28 after the community screening on 17-19 February, further reducing the number of sources of infection in the community (Fig.2). The modelling estimated 87% (lower bound, 53%) of the infections before 8 March 2020 were unascertained (potentially including asymptomatic and mildly symptomatic individuals) and the corresponding population infection rate was about 2.5%. Although the infectivity of undiagnosed infections is only half of that of confirmed cases in the model according to the literature, it may play an important role in propelling the early development of the epidemic due to their high proportion. In the later stage, due to comprehensive measures such as universal mask wearing and social distancing, the transmission route was effectively cut off. Although these infected persons were not diagnosed and isolated, their transmission capacity was greatly restricted, and its number gradually declined through self-healing (Fig. 2). A number of serological investigations published recently in European and American countries also found that the proportion of local populations with positive antibodies to the novel coronavirus was much higher than the proportion of confirmed novel coronavirus patients, which is basically consistent with the results of this study, and both reflect the high covertness of novel coronavirus infection. In addition, the results of a serological study published by the team of Academician Fanfan Hou of Southern Medical University in Nature Medicine on 5 June showed that the antibody positive rate among medical staff and their families in Wuhan and the employees of the hotel was 3.2-3.8%, but the actual infection rate in the general population needs to be confirmed by more extensive serological studies.
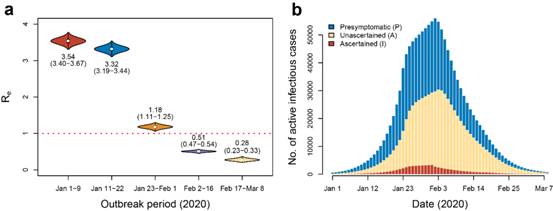
Fig. 2. The transmission characteristics of the novel coronavirus: (a) the effective regeneration coefficient at different stages; (b) the total number of daily active infectious cases and their composition.
Such high covertness and high transmissibility have greatly increased the difficulty of epidemic prevention and control, and also explained why it can spread rapidly around the world. Using model prediction, the study further assessed the possibility of resurgence of the epidemic caused by the lift of prevention and control measures under different conditions (Fig. 3). If 87% of infected persons are not detected and all prevention and control measures are lifted after 14 consecutive days of zero confirmed cases, the probability of a second outbreak is 32%. If only 53% of the infected are undetected, the corresponding probability of the resurgence will drop to 6%. Premature lift of prevention and control measures will greatly increase the possibility of a second outbreak of the epidemic. These results suggest that confronting the covertness of novel coronavirus, we should maintain epidemic monitoring while resuming work and production to restore economic order, and quickly adjust prevention and control measures based on changes in the epidemic to prevent secondary outbreak. These research results are of significant reference value for global epidemic prevention and control and the formulation of corresponding public health policies of all countries around the world.
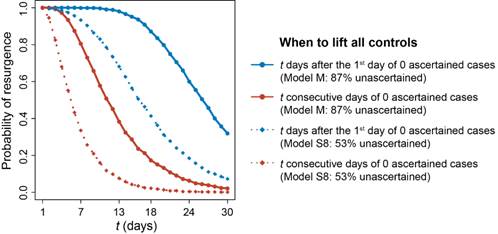
Fig.3: Risk of resurgence after lifting all controls under different assumed conditions
School of Public Health, Tongji Medical College, Huazhong University of Science and Technology is the first completing unit. Dr. Xingjie Hao, Associate Professor Shanshan Cheng and Dr. Degang Wu are all first authors. Professor Chaolong Wang, Professor Tangchun Wu, and Professor Xihong Lin from Harvard T. H. Chan School of Public Health are corresponding authors.
Link to the paper:
https://www.nature.com/articles/s41586-020-2554-8
